COVID-19 Bulletin: Friday 7 January
January 7, 2022
Numbers not statistics: This week (last week).
| Colleagues who have received COVID-19 1st Vac. | Colleagues who have received COVID-19 2nd Vac. | Colleagues who have received COVID-19 booster Vac. | Current number of confirmed COVID-19 inpatients | COVID-19 inpatients not vaccinated against COVID-19 | Total number of our patients who have died from COVID-19 |
| 84.04% (84.67%) |
79.64% (80.07%) |
32.06% (39.22%) |
186 (81) |
34.41% (53.09%) |
1,416 (1,402) |
(Note: Percentages may decrease due to changes in the number of inpatients and in the number of staff members (starters and leavers).
* Figure dropped due to data clean
1. New: Revised PPE Guidance: Important update
We have carried out a further risk assessment in relation to PPE usage in our clinical areas. This has taken into account the following:
- Current high volume of infection rates in the community
- The corresponding high number of COVID-19 admissions
- Some cases where patients on amber non-COVID wards have subsequently had a positive COVID PCR swab test after initial negative test
- Increasing outbreaks in our ward areas
- The ventilation in our ward areas (although new HEPA filters in Sandwell are helping with this).
The outcome of that risk assessment has led to a decision to increase the required level of PPE in these inpatient environments for some staff. This is above and beyond the current national guidelines. This is under constant review and may well change if the regular review of the risk assessment indicates that the risk is lowered.
For all inpatient areas where there is direct patient contact (in red and amber wards), staff should wear as a minimum:
- A silicone mask/FFP3 mask – these can be sessional use. Single use gloves and aprons (please ensure you have been fit tested for an FFP3 mask before use). Visors may be necessary in some clinical circumstances as per risk assessment for each individual patient.
- You should wear a fluid-resistant surgical face mask if you do not have direct patient contact. Non-direct patient contact includes walking on a ward area, pharmacists, clerical staff, estates and facilities staff. Disposable gloves/aprons should be worn for contact with patients/immediate environment. Porters who are transferring patients should wear FFP3/silicone face mask when transferring patients to red and amber wards.
- If you are visiting the ward from another area, a minimum requirement when entering the unit will be to wear a fluid resistant surgical face mask.
Please note: staff must follow their individual risk assessment for PPE. Occasionally this will recommend a higher level of protection depending on your individual assessment.
- For all outpatients and community staff inclusive of health visitors/school nurses/GP practices, for staff visiting care home facilities, patients and families homes, surgical face masks should be worn as a minimum with a disposable apron and gloves for direct patient care. Follow your individual risk assessment to see if you need a higher level of PPE.
- If clinical intervention is required, a clinical risk assessment should be undertaken prior to the contact to establish whether there is a requirement for a higher level of PPE. For example, if a patient with a known respiratory condition has a persistent cough (not COVID related), an FFP3 and a visor should be worn in the event that the contact is essential and cannot be delayed.
- Porters and facilities staff on wards can continue to wear a surgical face mask. However, if they are in direct patient contact, they will then need to follow the guidelines outlined above for inpatient staff.
- Fluid resistant surgical face masks may be worn in rest areas and managers are urged to ensure colleagues have regular hydration breaks. If you have any questions, please speak to your line manager or infection control on ext. 5900 or email swb-tr.SWBH-Team-InfectionControl@nhs.net.
You should be fit-tested for the current masks we have in stock but if you aren’t please make sure you do so as a priority. FFP3 masks can be obtained through usual arrangements by ordering from Stores. Fit testing continues at City Hospital, details of how to book are on Connect.
2. New: COVID-19 vaccination regulation: Get your first dose by Thursday 3 February
You will be aware that the Government are introducing COVID-19 vaccination as a condition of employment for all frontline health and social care workers. As a result, health and social care providers in England will be required to ensure workers are fully vaccinated (with dose 1 and 2) against COVID-19, unless they are exempt, under plans announced by the Health and Social Care Secretary.
It is expected that staff will be fully vaccinated by 1 April. This means that you will need to have had the first dose by 3 February at the very latest and the second by 31 March, unless you are clinically exempt.
Please note that at present, the regulations do not require evidence of boosters, although we continue to encourage you to take up the booster vaccination offer.
If you are in a role that requires you to be fully vaccinated, then you will not legally be able to undertake this role if you have not received both doses of the COVID-19 vaccines by 1 April.
We are working closely with key stakeholders to ensure that colleagues are communicated with on the above regulations. We will be writing to all staff for whom we do not have confirmation of their vaccination status.
We understand that colleagues may have queries in relation to the vaccine and would like to discuss your concerns in more detail. For any queries on vaccines such as suitability, effectiveness, any concerns about side effects, please contact occupational health on swbh.occyhealthcovidvaccine@nhs.net or telephone 0121 507 3306.
3. Updated: Testing and isolation for NHS staff
Recent government guidance has changed the arrangements for testing and isolation allowing some staff to return to work after being COVID-19 positive if they are well and have two consecutive negative lateral flow results from day 6.
The guidance on PCR testing for NHS staff has not changed despite the changes for the wider population. This is to protect patients within our care and other colleagues.
The staff isolation and when to come back to work information sheet is important as it includes information on what to do if you or one of your team members tests positive for COVID-19, or is in contact with a COVID-19 case. It also includes information on when PCR tests should be accessed, or faster turnaround tests of which there is a limited supply, and the definition of a “contact”.
As a summary:
- If you have COVID-19 symptoms and have a negative lateral flow test result , we still require you to have a PCR test with a negative result in order to come into work.
- If you have no symptoms but are a contact of a positive COVID-19 case but have tested negative on a lateral flow test, we still require you to have a PCR test with a negative result in order to come into work.
- PCR tests can be booked at Little Lane carpark, Sandwell Hospital, by calling the Contact Centre on 0121 507 2664 – option 6.
Please read the staff isolation and when to come back to work information sheet and share with your colleagues.
4. Updated: Unplanned admissions pathway
Colleagues are advised to review the unplanned admissions pathway which has now been updated.
You are alerted to:
- A change to the re-screening of positive patients on admission in the emergency department. If a patient has previously tested positive for COVID-19, they no longer need to be re-screened for 90 days from the first positive result. However, these patients may require retesting if they have new COVID symptoms.
- Patients who attend ED and who have had covid within the last 90 days and are asymptomatic need to go through the medium risk stream.
To review the pathway please click here.
5. Updated: Resource pack for managers – new guidance on employee wellbeing support
The COVID-19 Resource Pack for Managers has been updated. So what’s new?
Section 8: Employee Well-Being Support
New guidance added:
- Supporting staff suffering domestic abuse or violence
- Bereavement Practices – Understanding different bereavement practices & how our colleagues may experience grief.
If you are a manager, you must familiarise yourself with the COVID-19 Resource Pack for Managers as it is reviewed on a regular basis – see the latest version on Connect.
6. Reminder: Recording COVID absence in ESR
The guidance showing how you can record COVID related absences on ESR has now been updated and can be accessed by clicking here.
Note: Managers are reminded that they should not record an absence if the colleague is working from home and they must ensure that if a colleague is absent due to COVID that this is entered in the related reason field in ESR (see guidance for further information).
For more information please email s.sutton2@nhs.net.
7. Reminder: New treatment for COVID-19 patients
You may be aware we were administering Ronapreve, a neutralising monoclonal antibody (nMABs), which is a new type of COVID-19 treatment, usually given intravenously.
However, Ronapreve is not effective against Omicron which is currently the predominant COVID variant in patients admitted to hospital. Therefore it should no longer be prescribed to any patient.
We now are administering another nMABs therapy which is effective against Omicron, called Sotrivumab (Xevudy), which is specifically for patients with hospital-acquired COVID-19, who are aged 12 and above and weigh more than 40kg.
This drug can also be offered to high risk patients in the community, within five days of a positive PCR test. If you are in contact with eligible patients please ask them to call 111 or contact their GP. They will be referred to the newly formed COVID Medicine Delivery Unit (CMDU) based at City Hospital where the drug is being administered.
What are Neutralising Monoclonal Antibodies (nMABs)?
Monoclonal antibodies work just like the antibodies your body makes to fight viruses and other bugs, but are special because they are made in the labs of pharmaceutical companies. They are designed to target the coronavirus spike protein which sits on the outside of the virus and which the virus uses as a key to get into cells in the body.
Eligibility Criteria
- PCR positive COVID-19 test result received within last 72 hours.
- AND onset of symptoms within last seven days.
- AND a member of a highest risk group
- aged >12 years and >40kg
The high-risk group include patients with downs syndrome, sickle cell disease, solid cancer, haematological malignancy, severe renal and liver disease, decompensated liver disease, those on significant immunosuppression, primary immune deficiencies.
Further details about the new treatment can be found in the following guidance document: COVID Medicine Delivery Unit (Word)
Please continue to use the pathways in place for hospitalised patients as described in the following links:
- http://myconnect.swbh.nhs.uk/wp-content/uploads/2021/12/nMAB-in-Hospitalised-Patients-Pathway.pdf
- http://myconnect.swbh.nhs.uk/wp-content/uploads/2021/12/Initial-Assessment-of-Potential-COVID-19-Patients.pdf
8. Reminder: Start 2022 safely – get protected, get boosted
Make sure you start the New Year right by getting the most protection possible against COVID-19. More than three quarters of eligible adults have now received the lifesaving booster. That’s over 28 million people, making this the biggest and most successful vaccination drive in NHS history!
Those who are yet to receive their booster, or the first and second COVID-19 vaccinations, are strongly urged to do so as soon as possible.
Our vaccination centres are open seven days a week, here are the upcoming opening hours.
| Dates | Tipton Sports Academy Vaccination Centre (*walk-ins) | City, Sheldon Block (*walk-ins) | Sandwell, Berridge Suite (*walk-ins) |
| 7 January | 8am – 9pm (*8pm) | 8am – 8pm (*7pm) | 8am – 7pm (*6pm) |
| 8 January onwards | 8am – 7pm (*6pm) | 8am – 7pm (*6pm) | 8am – 7pm (*6pm) |
Note: You can also book a vaccine on the national booking website.
Here’s a short animated video of exactly what happens when you go for your jab.
Not had your flu jab? Get even more protected as you start the New Year. It’s safe to have the COVID-19 booster and the flu jab at the same time, just ask your vaccinator.
Have questions about getting the jab?
We will be holding some question and answer sessions where you can ask our panellists of senior clinical leaders about the vaccinations and how they protect us from serious disease.
Join in and ask your colleagues to come along too. Session dates and times are below:
| Date | Time | Joining instructions |
| Monday 24 January | 1pm – 2pm | Click here to join |
| Thursday 27 January | 3pm – 4pm | Click here to join |
| Friday 28 January | 11.30am – 12.30pm | Click here to join |
9. Reminder: Join the saliva testing programme to protect your patients and loved ones
All colleagues must do a weekly LAMP test. If you are not registered for LAMP you must do a lateral flow test twice a week. This is the national requirement and all staff must comply. With this in mind, please ensure you have adequate stock levels. Need to order lateral flow tests kits? Click here to order.
Did you know saliva testing (known as LAMP – Loop Mediated Isothermal Amplification) is a speedy and less invasive way of detecting COVID-19?
You can book a kit collection slot for the weekly test, which requires you to spit into a tube in the morning before you brush your teeth or an hour after you have eaten.
When you arrive at work, you can deposit your sample into a red collection box. Many of these are positioned around our acute and community sites.
You can find drop off points and more information by clicking here.
If you are still unsure how to complete your LAMP test, be sure to check out the step-by-step guide in the video below:
Even if you are vaccinated it is vital that you register and carry out the weekly tests as they will help identify if you’re asymptomatic. Your saliva sample is ONLY used to test for COVID and is disposed of after testing.
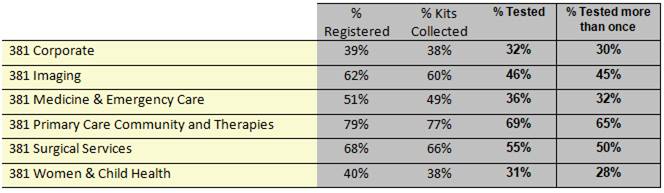
Uptake of the weekly saliva test is monitored to ensure we are doing everything we can to protect our patients, the public and each other.
The latest data by group is below:
10. Reminder: Looking after your mental health
It’s more important than ever that we look after ourselves, stay connected, and keep the conversation going about how we are feeling and how these circumstances are affecting us.
Black Country Healthcare NHS Foundation Trust (BCHFT) has set up a Black Country and West Birmingham Staff Mental Health and Wellbeing Hub, to provide an entry point into mental health talking therapies and support for colleagues across the Black Country and West Birmingham Integrated Care System (ICS).
Qualified mental health professionals offer priority pathways to confidential telephone, video, or face-to-face support tailored to individual needs, provided by local mental health teams and support services close to home.
Don’t suffer in silence: If you are feeling overwhelmed or need someone to talk to. If you feel that you would benefit from this support, you can self-refer by visiting the BCHFT website. Alternatively, you can email bchft.hub@nhs.net or call 0121 8031444.
Note: This is not a crisis service. If you require urgent mental health support, please call Rethink’s 24/7 mental health helpline on 0800 0086516 or visit BCHFT’s help in a crisis page for a range of options. You can find out more about the 24/7 mental health helpline here