Monthly archives: February 2022
Heartbeat: On a mission to a greener NHS

A nurse for over 30 years, Clare Nash, Head of Clinical Products Management at the Black Country Alliance is on a mission to influence and inspire her colleagues to make greener choices.
Speaking to Heartbeat she explained: “I love meeting and working with many clinicians across the acute and community sectors, and believe together we make great improvements in patient care. Being able to influence and implement the Greener NHS agenda is what gets me fired up each day though. I lead a regional greener care group that is implementing several net zero programmes of work on reuse of products including silicone tourniquets. We are also looking at how we might expand our reuse of walking aids, and implementing reusable theatre caps and gowns, and I am always looking for colleagues to share their ideas on what products we focus on next to go green.
“As a clinical procurement nurse I ensure the products we use to care for our patients and colleagues are safe, fit for purpose, sustainable, standardised, and deliver quality and value for our trusts, the taxpayer and the planet. Around 62% of NHS greenhouse gas emissions come from the products we procure for us to care for our patients. We have developed a Sustainability Impact Assessment for the Black Country ICS to measure any adverse and positive effects from the products we procure. We are already implementing greener solutions across the ICS, including reusable respirators in place of single use FFP3s, reusable non-sterile gowns, and type IIR surgical masks. This has reduced waste, ensured continuous supplies even at the height of the first wave of COVID, and saved precious planetary resources.”
As part of a wider procurement team across SWB and Dudley, Clare works alongside clinical colleagues to understand their needs, and source sustainable products that are fit for purpose whilst adhering to National Institute for Health and Care Excellence guidance and evidence-based practice.
The NHS uses 45 million single use tourniquets every year. Working with the critical care outreach team, Clare is currently evaluating a reusable wipeable tourniquet which she is hoping we will transition to if tests go well. Her focus on sustainability came after she had been working in clinical procurement for a few years when her current role was advertised, and seeing the positive impact she could have on patient care, she naturally jumped at the opportunity. Now, working across two Trusts, and leading a regional group, she supports more staff to deliver safer, greener care for patients.
Clare believes that we all should sign up to delivering greener care. She explained: “The climate emergency is a health emergency and every one of us has a role to play in getting to net zero and doing our patients no harm. Delivering on our regional programmes of work will contribute a significant reduction in carbon emissions and waste reduction, improve air quality, and deliver greater social value to our local communities.”
Tax avoidance: Don’t get caught out!

Tax avoidance is when people bend the rules of the tax system to try to pay less than they owe. HMRC’s report, the Use of Marketed Tax Avoidance schemes in the UK, has shown that contractors are often targeted and drawn into schemes marketed by companies promising higher take home pay and less administration. Many of these schemes do not work and there could be significant financial implications for anyone involved. Use the risk checker to check whether your current contract could involve tax avoidance.
You don’t need to be a tax expert to spot an avoidance scheme. If you’re offered higher take home pay simply for rearranging how it reaches you, for example as a non-repayable loan or as a trust payment, it almost certainly is tax avoidance.
Look out for any of the following signs:
- A scheme that allows you to keep more of your income than you would expect, with little or no deductions for Income Tax and National Insurance contributions (NICs)
- Some, or all of the payments are said to be “non-taxable”. These could be described as loans, annuities, bonuses, or shares. These payments are no different to normal income and you still need to pay Income Tax and NICs on them
- You may be told the schemes are safe and compliant or approved by HMRC. This is not true - HMRC never approves avoidance schemes
- Only a part of the total payments you receive are taxed as income. If you are employed, this is often close to the national minimum wage
- You are offered a choice between a standard or “enhanced” pay scheme. The enhanced version is likely to be tax avoidance
- You have been asked to sign more than one contract or agreement
- Your employment contract or agreement does not state how your income will be paid, or provide you with a breakdown of all your deductions
- You may even be offered a ‘cash bonus’ if you recommend the scheme to a friend.
Recognise tax avoidance. Learn how to spot the signs, understand how it works, and know the risks.
Understand how umbrella companies work. If you work through an ‘umbrella company’ – here’s what you need to know about how they should operate.
Check your pay and contract arrangements. Looking at your payslip is a useful way to check for signs that you may be involved in a tax avoidance scheme.
Get help if you think you’re already in a tax avoidance scheme and don’t know how to get out.
If you think you have spotted a tax avoidance scheme, you can report it by using the Report Tax Fraud Online form. Please make sure you enter the words ‘Contractor campaign’ in the ‘Other information’ section. You can also phone HMRC on 0800 788 887 (outside the UK +44 (0)203 080 0871).
If you think you are in a tax avoidance scheme, contact the team and the will help you get on the right track. They won’t be judgemental and if you can’t afford to pay everything in one go, they may be able to offer you an instalment arrangement. Email exitsteam.counteravoidance@hmrc.gov.uk
For further information read Tax avoidance: getting out of an avoidance scheme.
Star of the Week: Marie Matthie
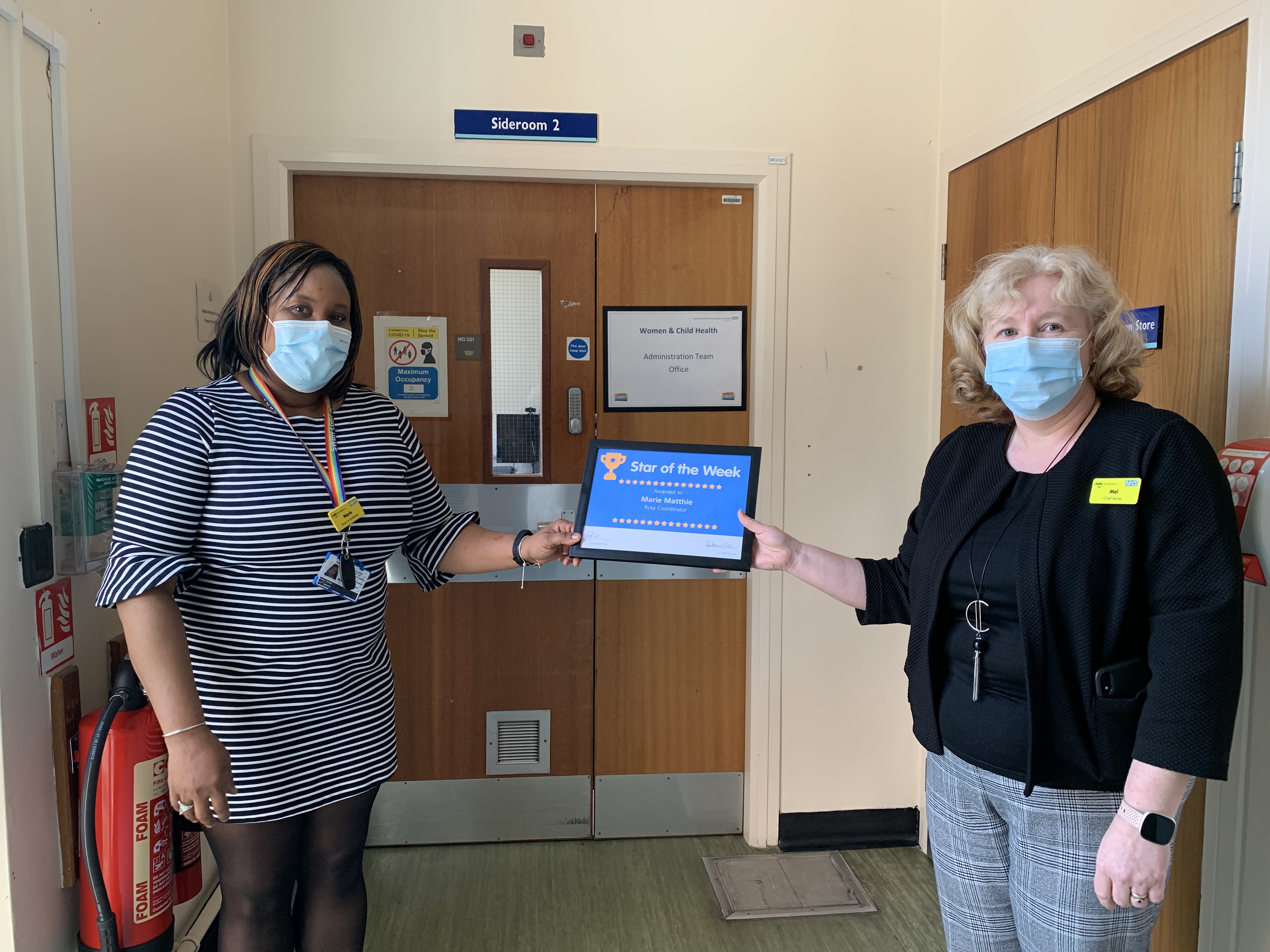
Our Star of the Week is Marie Matthie, Rota Coordinator for Women’s and Child Health.
Marie’s role involves ensuing the consultant and junior doctors rotas are covered within Women’s and Child Health. Due to COVID her role has become monumental to ensure all clinical aspects of the ward areas are covered to ensure patients received their care but despite this, Marie continues to work to exceedingly high level ensuring all tasks are complete. Marie has had extra pressures in ensuring shifts are covered due to COVID and increased sickness within our areas but has still completed all her work to a satisfactory level. Marie ensures all rotas are consistently monitored and kept update on all the relevant systems used. Marie is hard working and always gives 100 per cent.
Do you know someone in your team that has gone above and beyond the call of duty? Why not put them forward for Star of the Week by clicking here.
Star of the Week: Marie Matthie
Our Star of the Week is Marie Matthie.
Marie’s role involves ensuing the consultant and junior doctors rotas are covered within Women and Child Health. Due to COVID her role has become monumental to ensure all clinical aspects of the ward areas are covered to ensure patients received their care but despite this, Marie continues to work to exceedingly high level ensuring all tasks are complete. Marie has had extra pressures in ensuring shifts are covered due to COVID and increased sickness within our areas but has still completed all her work to a satisfactory level. Marie ensures all rotas are consistently monitored and kept update on all the relevant systems used. Marie is hard working and always gives 100 per cent.
Do you know someone in your team that has gone above and beyond the call of duty? Why not put them forward for Star of the Week by clicking here.
Chief Executive’s Message – Friday 11 February

Hello colleagues
There have been many positives that have occurred as a result of the pandemic, in my opinion. Those positives include things like a greater societal understanding that social care is separate from health care and equally important; the speed at which the NHS and its staff responded to the crisis, abandoning bureaucracy to deliver quick change; the focus on staff health and wellbeing which now cannot be reversed.
However, the pandemic and its impact has also been very negative. Beyond the obvious untold damage it has done to families and communities who have lost loved ones, it has also brought with it as a bi-product, deepening health and economic inequality, a concerning decrease in civility between humans, in mutual respect, in tolerance and understanding. This manifests itself in, just to name a few:
- Intolerance of adhering to IPC expectations by the general public
- Increased aggression and violence towards our colleagues in clinical services
- Lack of respect shown to medical secretaries, call centre and admin colleagues by the general public who are concerned about lengthy waiting times
All of these are worrying enough, but our concern should be further compounded when we see or hear of examples in which our own colleagues are intolerant and disrespectful to both members of the public, to patients, to carers or even to each other. I am afraid to say, whether it is because my senses are heightened at the moment, or whether its because there really has been a deterioration in the conduct of some, I feel it and I have got involved myself, in this kind of stuff with increasing frequency.
To illustrate, local residents near Sandwell General Hospital have complained about staff making noise and littering their streets. We have one of our main sites in a strongly residential area. We must respect that and consider what we would want if we lived on Hallam Street or Lyndon, for example. I am also concerned that the journey to respecting others starts with self respect and that starts with self presentation. Some colleagues have left their dress code and uniform standards slip during the pandemic and far too many staff are wearing scrubs and uncovered uniforms outside of Trust premises and even in shops and on public transport.
We need a post-pandemic reset on so many fronts, not least staff wellbeing, elective recovery, refocused Trust strategy. We also need a reset on how we treat each other – our values, in other words. We will be agreeing a new, shorter list of organisational values, with your help and support, over the next few weeks as part of that reset. I’d be amazed if colleagues didn’t think that civility and respect would be in that final list in some way, shape or form. Civility is important. Civility can save lives. See the research here:
https://www.civilitysaveslives.com/
Have a good week
Richard
Do you know when you are moving to Sharepoint?

By the end of February all clinical and non clinical wards, departments and operational teams across our organisation will need to have moved all of their data and working practices away from shared drives and network shares and be fully migrated over to Office 365.
This means all staff should now know when their area is scheduled to move to Office 365, and if you haven’t yet been told, please take the time to speak to your line manager.
The move to Office 365 is being carried out gradually, with departments organising their migration dates, informing their staff and working with colleagues in informatics to ensure that all of their current computers are compatible with the new system.
But if you are unsure of how the move should be organised, here are some pointers:
How does a migration to Office 365 work?
- Wards, teams and departments are responsible for planning their migration date – with migrations planned to be completed by the end of February.
- Departments to organise a nominated lead to prepare their data for migration. This lead should get in touch with informatics and agree which networks shares they will be responsible for.
- Nominated lead to discuss their requirements with informatics including discussing any issues they feel might affect their ability to operate their department. This should include testing to ensure that all of their working practices and systems continue to work on Sharepoint and Office 365.
- All staff to ensure they have working NHSmail logins and are able to access Office 365 online at https://www.office.com
- Nominated lead (with support from IT where requested) to migrate their data to Sharepoint and to communicate with their team when they need to stop storing and accessing files on network shares and begin using Sharepoint.
- Once migration is complete, network shares will be disabled.
Please take the time to plan, discuss and begin carrying out your migrations as soon as possible. Further information can be found on Connect, and support can be sought from colleagues in informatics by contacting ext 4050 or by emailing: swbh.sharepoint.migration@nhs.net
Share your feedback on revoking vaccination as a condition of deployment across all health and social care
Colleagues will be aware about a review of the Vaccination as a Condition of Deployment legislation. The Secretary of State for Health announced in parliament on 31 January that the legislation is being reconsidered. The Government’s decision is subject to a parliamentary process and requires further consultation and a vote to be passed into legislation.
The consultation is now open and is seeking views on the government’s intention to revoke regulations that would make vaccination a condition of deployment for all healthcare workers.
If you wish to take part in the consultation and give your feedback, please click here.
Please be aware that the deadline for feedback is Wednesday 16 February.
National Apprenticeship Week

This week is National Apprenticeship Week. The annual week-long celebration of apprenticeships aims to shine a light on the amazing work being done by employers and apprentices across the country.
To celebrate the awareness week, we will be promoting and sharing content about our apprentices and their fantastic contributions and efforts.
Be sure to check out this short video featuring Ryan Singh Lallie, Business Administrator talking about his apprenticeship role on Lyndon Ground.
Want to get in touch with our apprenticeship team? This week each member of the team will have a dedicated timeslot where you can catch up and have an informal chat about anything apprenticeship. Also be sure to get involved with the theme of day!
| Thursday 10 February – thank you Thursday | Helen Colbourne – Non-Clinical Apprenticeship Co-ordinator | 11am – 1pm | 07790 601269 |
| Julie Smith – Senior trainer | 11am – 1pm | 07970 882516 | |
| Friday 11 February – celebration Friday | Karen Whitehouse – Apprenticeship Coordinator | 11am – 1pm | 07976 075466 |
| Saturday 12 February – Parents/carers including Selfie Sunday | Karen Whitehouse – Apprenticeship Coordinator | 9am – 11am | 07976 075466 |
If you are interested in any degree and higher level apprenticeships, please take a look at what is available by clicking here and if something is of interest please contact swbh.apprenticeship@nhs.net for the next steps.
DID you know…? Only 12% of patients in September had their nursing needs assessed using the SCP template
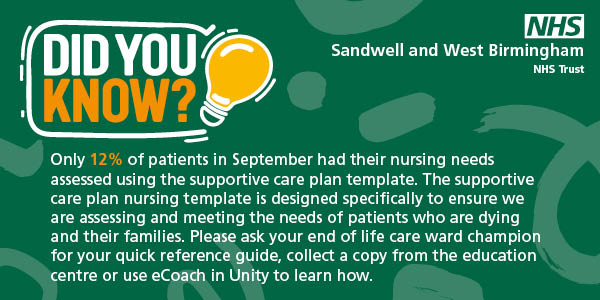
The SCP nursing template is designed specifically to ensure we are assessing and meeting the needs of patients who are dying and their families. Please ask your end of life care ward champion for your quick reference guide, collect a copy from the Education Centre or use eCoach in Unity to learn how.
Initiation of the Supportive Care Plan (SCP) is done by the medical team responsible for the patient’s care by populating the initial medical assessment in the workflow, including medical condition, patient and family’s understanding and wishes for the future including preferences about onward care. There will then be a flag assigned to that patient highlighting the need to ensure excellent supportive and palliative care.
Nursing care should then be documented using the SCP shift assessment to guide symptom assessment and family/carer support in the same workflow. SCP ward round notes will then pull info from nursing shift reviews and reviews to keep information together and reduce time inputting information.
For more information see the connected palliative care pages. For training, use eCoach in Unity or collect your quick reference guide either from your end of life care champion on your ward, or from the Education Centre.
COVID-19 Bulletin: Thursday 10 February

Numbers not statistics: This week (last week)
| Colleagues who have received COVID-19 1st Vac. | Colleagues who have received COVID-19 2nd Vac. | Colleagues who have received COVID-19 booster Vac. | Current number of confirmed COVID-19 inpatients | COVID-19 inpatients not vaccinated against COVID-19 | Total number of our patients who have died from COVID-19 |
| 90.78%
(89.27%) |
85.58%
(83.90%) |
51.22%
(50.78%) |
114
(139) |
34.21%
(31.88%) |
1,471
(1,462) |
Note: Percentages may decrease due to changes in the number of inpatients and in the number of staff members (starters and leavers).
- New: The correct PPE will help to curb infection rates
It remains important that all colleagues continue to follow the Trust’s PPE guidance as the number of patients with community acquired COVID-19 who become positive on admission remains high.
We all need to play our part in ensuring the correct equipment is worn, whether you are working within a red, amber or green clinical area, or in a non-clinical space.
As you may recall we enhanced our PPE requirements having risk assessed COVID-19 infection rates and outbreaks within our hospital ward areas. This guidance continues to remain in place.
Here is a reminder of the requirements:
For all inpatient areas where there is direct patient contact (in both red and amber/green wards), clinical and non-clinical staff who are having patient/bed space contact should wear as a minimum:
- A silicone mask/FFP3 mask – these can be sessional use. Single use gloves and aprons (please ensure you have been fit tested for an FFP3 mask before use). Visors may be necessary in some clinical circumstances as per risk assessment for each individual patient.
- You should wear a fluid-resistant surgical face mask if you do not have direct patient contact. Non-direct patient contact includes walking on a ward area, clerical staff, estates and facilities staff. Disposable gloves/aprons should be worn for contact with patients/immediate environment. Porters who are transferring patients should wear FFP3/silicone face mask when transferring patients to red and amber wards.
- If you are visiting the ward from another area, a minimum requirement when entering the unit will be to wear a fluid resistant surgical face mask.
We have also made the wearing of surgical masks mandatory for all inpatients and outpatients. This means that all patients must wear fluid resistant surgical masks whilst they are under our care. Masks do not need to be worn whilst patients are sleeping, eating or drinking. Exceptions are for patients who are under clinical exemptions. Other exceptions include women in labour, patients without capacity, including those who are not able to put on or take off their own mask, and for children under the age of 12.
Staff must follow their individual risk assessment for PPE. Occasionally this will recommend a higher level of protection depending on your individual assessment.
We will continue to risk assess our infection prevention and control guidance regularly in light of changing COVID-19 restrictions, hospital rates, outbreaks and community infections.
Do you need a disposable FFP3 masks?
- If you require disposable FFP3 mask please call ext. 4938 (City) or ext. 2824 (Sandwell).
- If you are in charge of a clinical area, please ensure you have an ample supply of these masks.
Note: We must remind colleagues they should not be reliant on their silicone mask only.
If you have not been fit tested for a disposable masks please book an appointment via ESR. If you have issues booking through ESR, please call ext. 5195.
- New: Keeping the channels of communication open between patients and their loved ones
Whilst visiting restrictions still remain in place, colleagues should continue to ensure that patients on their wards are given support in communicating with their loved ones.
You can do this by using the available iPads and mobile phones. If you don’t have this equipment, then please contact IT on ext 4050 to request devices.
Keeping the channels of communication open between patients and their relatives is an important element in helping to aid their recovery and also in supporting with their mental health whilst they remain in our care.
Visiting restrictions remain in place to protect patients and staff and is reviewed on a regular basis.
The current guidance is below:
- Visiting remains in place for vulnerable patients, those patients who are at the end of life, those with limited mental capacity and a parent/guardian supporting their child.
- Birthing partners are allowed to accompany a woman who is in established labour. The partner will need to provide evidence of a negative lateral flow test taken that day. Once a negative result is obtained they will be allowed into the Delivery Suite. Partners can currently continue to accompany the mum-to-be to any appointments and scans. Visiting on inpatient wards in our maternity department is limited to partners or birthing partners only for one hour a day. Loved ones should call the ward to arrange their visiting time.
- Vulnerable patients attending our emergency or outpatient departments can be accompanied by one person.
- Where visiting is allowed in exceptional circumstances, please ensure that this is agreed with the ward, is limited to one visitor and crucially that they are able to evidence a negative lateral flow test from that day and do not have any COVID-19 related symptoms.
- New: COVID-19 vaccines: read up on the facts
Vaccines against COVID-19 have been developed quickly – but they have been developed with great care.
Working together, doctors and scientists have analysed the results of trials. Yet still there remains a great deal of misinformation around the vaccines – whether it’s shared through social media, WhatsApp groups, or through the media.
It’s important that we help to educate those around us with the right information about the vaccines which are there to protect us against this deadly virus.
Imperial College London has developed an informative document which details the facts about vaccines, including information around immunity and pregnancy.
You can read the document in full by clicking here.
- Updated: Drop-in vaccination clinic at Rowley Regis Hospital
A drop-in vaccination clinic will take place at Rowley Regis Hospital on Thursday 17 February, 9am-4pm on the Westwood ward. The vaccination hub will be administering first, second and booster does of COVID-19 vaccines plus third doses for individuals aged 12 years and over with severe immunosuppression. The clinic is open for all colleagues and members of the public. You can also get your flu jab – it’s not too late.
If it’s more convenient for you to access City Hospital or Tipton Sports Academy, the vaccination clinics are open every day between 8am-6pm for walk-ins. You can also book an appointment between 8am-7pm by calling the vaccination hub on 0121 507 4404.
Act now and keep yourself safe. Visit a vaccination hub or drop-in clinic to get your flu jab and COVID-19 vaccinations.
- Reminder: Supporting your wellbeing at work – Does your staff rest area need a refresh?
You will have seen in Tuesday’s COVID-19 bulletin, the many services offered to support your health and wellbeing. Having a comfortable place to relax and rewind during our breaks at work is just one of the areas we are looking to improve.
So, does your staff rest area need a refresh? If it’s looking a little tired or could do with a fresh lick of paint or a furniture upgrade, let us know. We are happy to consider requests for new furniture or equipment to improve rest areas and also requests for minor works such as painting and shelving. If your rest room needs a freshen up, please complete the Staff Rest Room Refresh Request Form (Word) and email it to Dinah McLannahan, Chief Finance Officer (dinah.mclannahan@nhs.net). She will then get in touch to progress your requests.
- Reminder: Be a cleaning champion
The Cleaning for Confidence campaign, led by the Midlands’ Nursing and Workforce team, helps to stop the spread of COVID-19 by encouraging colleagues to become cleaning champions with a 20-minute e-learning programme designed to further their knowledge of good cleaning practice.
Keeping NHS premises safe and clean for our patients is a key and shared commitment, and this has never been more important than now. A clean workplace is our first and best defence in stopping the spread of COVID-19 and other infections. Every person within the NHS family has a part to play in maintaining that commitment to keeping people safe.
Take a few minutes to access the Cleaning for Confidence e-learning programme here. The programme promotes further knowledge of good cleaning practice and the personal precautions needed to ensure the risk of environmental transmission both for patients and staff is reduced. This aims to help stop the spread of COVID-19 and, as always, reinforcing other behaviours that can help minimise the outbreak of other infections.
- Reminder: Regular testing is still important
Although restrictions may have eased, working within the healthcare sector still means we may come into contact with vulnerable people, colleagues and the general public. It’s important we do our bit to keep everyone safe from COVID-19, and we can do so through regular testing. Thank you to all colleagues who continue to do a weekly LAMP test. Even if you are vaccinated it is vital that you register and carry out the weekly tests as they will help identify if you’re asymptomatic. Your saliva sample is ONLY used to test for COVID-19 and is disposed of after testing.
If you are not registered for LAMP you must do a lateral flow test twice a week. This is the national requirement for all staff. With this in mind, please ensure you have adequate stock levels. Need to order lateral flow tests kits? Click here to order. There are seven lateral flow tests per box, per order, to your household address.
If you are still unsure how to complete your LAMP test, be sure to check out the step-by-step guide in the video below.
Please be aware that as of 14 February, any colleagues registering for LAMP testing or those who are collecting new kits, will get labels rather than a request form.
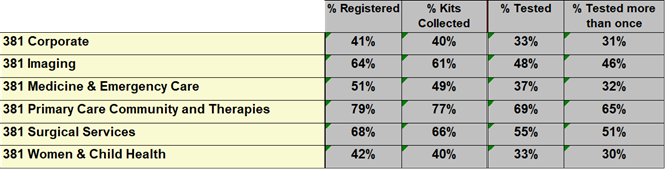
The latest data by group is below:
← Older items Newer items →
